One of the most common issues we confront when called to perform a physician billing department assessment, or a more broad-based medical practice analysis, is the lament: “Why aren’t we collecting more of our accounts receivable”. And the corollary: “Why can’t I get a straight answer to that question from the office manager/administrator/billing supervisor?”
When we ask questions about medical accounts receivable, we usually get answers like, “Oh, our AR is very low!” or, “Our AR is $XX”, with no way to tell if that’s good, bad, or ugly.
One of the reasons straight answers are hard to come by is that many staff members responsible for managing the medical billing process don’t know the relevant benchmarks and metrics to use for measuring accounts receivable performance. So they fall back on generalities or dollar amounts with no context. No wonder physicians and other healthcare providers are skeptical and frustrated.
Medical Practice Revenue Cycle: a Best Practices Checklist
In fact, it’s fairly easy to monitor the overall performance of your accounts receivable efforts, and looking at these measures each month can provide an early warning of potential collection problems – and the effect on cash flow. It’s also part of the best practices in medical billing you need to implement, even if your cash flow seems adequate right now. So, as a practice owner or manager, it’s critical to have a handle on your medical accounts receivable. Here’s exactly what you need to know.
Measuring Medical Accounts Receivable: “Days in AR”
The first measure is the “days in accounts receivable” – the average number of days it takes to collect the payments due to the practice. To calculate days in AR,
- Compute the average daily charges for the past several months – add up the charges posted for the last six months and divide by the total number of days in those months.
- Divide the total accounts receivable by the average daily charges. The result is the Days in Accounts Receivable.
total charges for last 6mo / number of days in last 6mo = average daily charges
total AR / average daily charges = days in AR
For instance, if you have charged $280,000 in the past six months, and if there were 182 days in those months, your average daily revenue is $1,538. Then, if your total accounts receivable is $70,000, the Accounts Receivable Days is 45.5. It is taking an average of 45.5 days to collect your payments.
$280,000 / 182 = $1,538
$70,000 / $1,538 = 45.5
So is that good? Well, Medicare usually pays about 14 days after receiving a claim. Some HMOs pay claims at 45 days after receipt, the time allowed by law in some states. We look at the following figures as benchmarks for medical billing and collections:
- 30 days or less for a High performing Medical Billing Department.
- 40-50 days for an Average performing Medical Billing Department.
- 60 days or more for a Below Average Medical Billing Department.
Measuring Medical Accounts Receivable: “Aging Buckets”
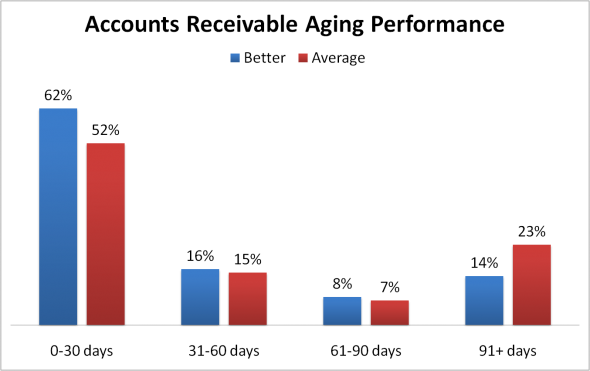
The other measure is the percent of accounts receivable in each “aging bucket”, for instance, 0-30 days, 31-60 days, 61-90 days, etc. To calculate it, you will need a report showing the dollar amount of the AR in each aging bucket. Simply convert each bucket to a percent of the total AR. The graph below shows the contrast between Better-performing billing departments vs. Average-performing billing departments.
Take a look at our presentation on “A Better Physician Billing Department“. There you’ll find more information on benchmarks, and questions to ask a billing department. And if you’re hesitant to seek outside help, take a look at our Case Studies and ROI to get an idea of how investing in the services of a qualified medical billing consultant can pay off handsomely.


Comments are closed.